
Healthcare operations are under pressure like never before. Patients expect the speed and convenience of apps and digital banking, but too many workflows still rely on manual phone calls, after-hours charting, and paperwork delays that push care back days or weeks. Trust me- despite the large million dollar machines, healthcare is one of the most manual industries ever.
91% of U.S. healthcare leaders say manual processes are their biggest operational bottleneck, while 65% of organizations confirm revenue cycle management remains heavily manual despite years of digitization efforts.
I’ve worked with ops teams who tell me the same story: the system isn’t broken because of bad people-it’s broken because of repetitive work that steals time from actual patient care.
AI agents in healthcare are changing that. They’re not here to replace clinicians or take over hospitals. They’re becoming the operational safety net that handles scheduling gaps, intake friction, follow-up reminders, and prior authorization prep-so staff can focus on what only humans can do: build trust, make judgment calls, and deliver empathy.
This guide is for healthcare ops leaders. It shows you what’s already working (real use cases), where generative AI delivers ROI fastest, and how AI agents make patient care more convenient without the hype. The goal isn’t disruption. The goal is throughput: more patients seen, fewer delays, happier staff.
Key Terms (What Ops Teams Actually Need to Know)
AI Agents in Healthcare
Software that doesn’t just answer questions but takes action: schedules appointments, updates records, triggers reminders, gathers documents, and escalates when needed. Think of it as a digital team member who never sleeps.
Generative AI (GenAI)
Tools that create text, video, and images: draft notes, simplify instructions, summarize charts. In healthcare ops, this means turning complex info into clear patient messages or admin handoffs.
Ambient AI Scribes
Listens to clinician-patient conversations (with consent), drafts notes, and feeds them into your Electronic Health Record (EHR) system. This is one of the fastest-growing categories because documentation eats 2+ hours daily from most clinicians. (source)
Workflow Automation
When AI agents connect to your CRM, EHR, or scheduling systems to move work forward automatically-reducing manual steps between intake, visit, and follow-up.
Where AI Agents Are Already Working in Healthcare Ops (Today)
Healthcare ops teams are already using AI-not in sci-fi diagnosis, but in the daily friction that delays care. Here’s what’s live across hospitals, clinics, and health systems.
Patient Access: 24/7 Scheduling Without Missed Calls
Phone lines are still the front door for most healthcare. AI voice agents handle:
- Appointment booking and rescheduling
- Eligibility verification
- Basic intake questions (“Do you need a referral?”)
- After-hours coverage so patients don’t wait until morning
Real impact: Call abandonment drops 30–50%. Patients get scheduled same-day instead of “call back tomorrow.” Staff stop playing phone tag.
Clinical Documentation: Freeing Clinicians from After-Hours Charting
Ambient AI scribes listen to visits, draft structured notes, and push them into Epic, Cerner, or your EHR. Clinicians review and sign-no more typing at night.
Real impact: One large health system reported clinicians saving 2 hours daily. That’s capacity for 2–4 more patients per provider per day.
Revenue Cycle: Prior Auth and Claims Friction
AI agents pull clinical notes, assemble prior authorization packets, check eligibility, and flag missing pieces. When denials happen, they draft appeals with the right documentation.
Real impact: Turnaround time drops from weeks to days. Denial rates fall because submissions are complete from the start.
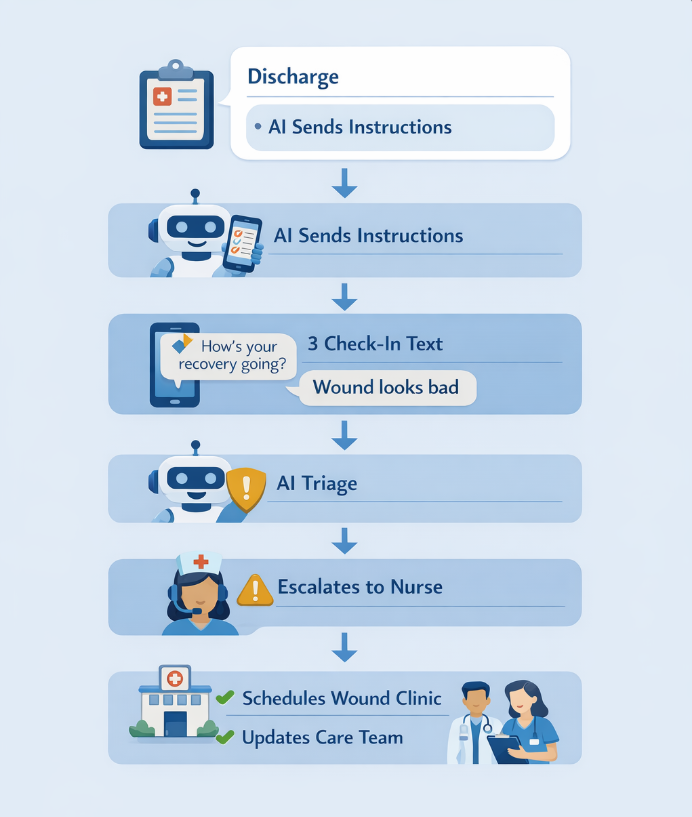
Care Coordination: Post-Discharge and Chronic Care Follow-Ups
AI agents send personalized discharge instructions, medication reminders, and check-in texts. High-risk patients get escalated to care managers automatically.
Real impact: Readmission rates drop. Patients feel “taken care of” instead of abandoned post-visit. It adds more empathy to healthcare.
Generative AI Use Cases in Healthcare Ops (The Fastest ROI Wins)
Generative AI isn’t magic. It’s an engine that turns messy healthcare communication into clear, actionable work. Here are the ops workflows where it delivers most.
1) Patient Instructions That Patients Actually Understand
Discharge papers are notoriously unreadable. GenAI rewrites them in plain language, personalized to the patient’s condition, medications, and reading level. Faster prescriptions for the doc, and better experience for the patient.
Before: Walls of medical jargon patients ignore.
After: “Take 1 blue pill twice daily with food. Refill reminder text goes out on the 20th.”
Ops win: Fewer “I didn’t know” callbacks. Better compliance. Happier patients.
2) Handoff Summaries Between Teams
GenAI reads charts and visit notes, then creates 1-page summaries for the next shift, specialist, or care manager: “Key issues, meds, pending tests, social barriers.”
Ops win: Reduces “lost in shift change” errors. Everyone starts with context.
3) Prior Authorization and Appeals Documentation
GenAI extracts medical necessity details from unstructured notes and builds compliant submission packets. When denials come back, it drafts appeals with supporting evidence. Modification controls are added to ensure no meaning ever changes.
Ops win: Cuts weeks off revenue cycle delays. Reduces coder burnout.
4) Staff Training and Onboarding Materials
New hires drown in policies. GenAI creates customized quick-reference guides and answers policy questions instantly. Even video explainers, policy walkthroughs, etc. can be generated through LLMs.
Ops win: Faster ramp-up. Less manager time spent on repetitive training.
Use Case Priority Matrix
| Workflow | Time Saved | Risk Level | Implementation Time |
| Patient instructions | High | Low | 1–2 weeks |
| Handoff summaries | High | Low | 2–4 weeks |
| Prior auth packets | Very High | Medium | 4–6 weeks |
| Staff training | Medium | Low | 1–3 weeks |
AI Agents in Healthcare: Your Digital Ops Team (The Game Changer)
Here’s where healthcare ops transforms: AI agents don’t just write-they execute.
A chatbot answers “What’s my balance?” An AI agent:
- Looks up the patient in your EHR/CRM
- Checks insurance and outstanding amounts
- Texts the answer + payment link
- Logs the interaction
- Escalates to billing if over $500
That’s not “customer service.” That’s end-to-end workflow automation.
Front Desk Agent (Patient Access)
What it does:

Ops impact: 24/7 coverage. Zero missed calls. Patients book without waiting.
Care Coordination Agent (Post-Discharge)
What it does:
Ops impact: Fewer readmissions. Patients feel continuously cared for.
How AI Agents Make Patient Care More Convenient (The Real Win)
Healthcare ops isn’t just about efficiency-it’s about experience. Here’s how AI agents deliver patient convenience without sacrificing safety.
Patients Get Answers 24/7
No more “office closed until 9 AM” voicemail. Patients text or call anytime:
- “Can I take this med with my allergy?”
- “When do I get my test results?”
- “How do I prep for my colonoscopy?”
AI responds instantly or escalates smoothly.
Fewer “Lost in the System” Moments
Patients hate repeating themselves. AI agents carry context across calls, texts, visits:
Monday: Patient calls about knee pain → AI books ortho → Gathers history
Wednesday: Ortho visit → Same history auto-populates
Friday: Follow-up text → Same agent recognizes patient
Clear Next Steps, Every Time
AI eliminates “I don’t know what to do” moments:
- Post-visit: “Here’s exactly what to watch for. Text us if this happens.”
- Pre-visit: “Bring these 3 things. Park in Lot B.”
- Med changes: “Your new prescription texts you reminders.”
The Emotional Multiplier
When ops work flows smoothly, clinicians aren’t burned out. They have energy for empathy, teaching, relationship-building-the human moments that actually heal.
The Path to Full AI Incorporation: 4 Phases Ops Can Plan For (Detailed Roadmap)
Healthcare won’t flip to “AI-first” overnight. It builds incrementally, each phase stacking on the last, unlocking more operational capacity while maintaining safety and trust. I’ve seen ops teams get stuck when they try to jump straight to “fully autonomous agents.”
The reality is more deliberate- and far more effective. Here’s what each phase actually looks like, with real workflow examples, implementation steps, success metrics, and pitfalls to avoid.
Phase 1: Assist (Today-2026): “AI as Drafting Copilot”
What it looks like in practice: This is where most healthcare organizations live right now. AI handles the cognitively heavy but repetitive text work, always requiring human approval.
Real workflows:
- Clinical Documentation: Patient visit → AI listens (ambient scribe) → Drafts SOAP note → Clinician edits/signs → EHR
- Patient Communication: Discharge → AI drafts plain-language instructions → Nurse reviews → Patient portal
- Prior Auth Prep: Clinical order → AI summarizes medical necessity from chart → Coder adds final details → Submits
Why it works: Zero risk to patient safety. Immediate time savings. Builds clinician familiarity.
Success metrics:
- Minutes saved per encounter (target: 5–15 min)
- Documentation completion rate (target: 95%+ same day)
- User adoption (target: 70%+ of clinicians using weekly)
Common pitfalls:
- Trying to automate too much too soon (e.g., auto-posting notes without review)
- Poor integration (AI outputs stuck in email instead of EHR)
- No measurement (can’t prove ROI, adoption stalls)
Transition trigger: When 70%+ of staff say “this saves me real time” AND you have clean audit logs.
Phase 2: Automate Repetitive Steps (2026–2027): “AI Handles Defined Tasks”
What it looks like in practice: AI agents take ownership of complete, low-risk tasks end-to-end, but humans still oversee outcomes and exceptions.
Real workflows:
- Appointment Scheduling Agent: Patient calls/texts → AI verifies identity → Checks eligibility → Finds slots → Books → Updates EHR → Sends confirmation → Alerts front desk
- Medication Reminder Agent: Day 3 post-discharge → AI texts “How’s the pain med working?” → Patient replies → AI logs response → Escalates abnormal symptoms to nurse
- Eligibility Agent: New patient inquiry → AI pulls insurance → Verifies coverage → Texts result + copay estimate → Escalates complex cases to billing
Key characteristics:
- Clear inputs → clear outputs: Patient said X → AI does Y
- Human oversight baked in: Every action logged, reviewable
- Escalation rules: “If patient mentions chest pain → immediate nurse callback”
Success metrics:
- Task completion rate without human intervention (target: 80%+)
- Patient satisfaction (target: NPS > 70)
- Error/escalation rate (target: <5%)
Common pitfalls:
- Over-automation (trying to handle complex cases too early)
- Weak escalation (patients feel “trapped” in AI loop)
- No feedback loop (can’t learn from escalations)
Transition trigger: When 80%+ of automated tasks complete successfully AND staff trust the escalation logic.
Phase 3: Orchestrate Workflows (2027–2028): “AI Coordinates Between Teams”
What it looks like in practice: Agents don’t just complete tasks—they connect them into seamless workflows across departments and systems.
Real workflow example (Patient Journey Orchestration):
- New patient inquiry (9 PM) → Access Agent books appt → Updates EHR
- 48 hours pre-visit → Prep Agent texts instructions + confirms attendance
- Check-in → Triage Agent gathers symptoms → Routes to right provider type
- Post-visit → Care Coordination Agent sends instructions → Schedules follow-up → Alerts high-risk patients to case manager
- Day 7 → Revenue Agent checks billing → Initiates prior auth if needed
What makes this phase powerful: Each agent knows only its piece, but together they create “one patient experience.” Front desk → clinician → billing → care manager all stay synchronized. No human has to “chase” between systems. Patient feels continuously cared for, not dropped between steps.
Technical requirements:
- Deep EHR/CRM integration (read + write access)
- Agent orchestration layer (workflow engine)
- Cross-agent context sharing (same patient ID across all agents)
Success metrics:
- End-to-end workflow completion rate (target: 85%+)
- Time-to-resolution across journey (target: 50% faster)
- Cross-department handoff errors (target: <2%)
Common pitfalls:
- Siloed agents (no workflow coordination)
- Integration debt (manual workarounds between systems)
- Scope creep (trying Phase 4 capabilities too early)
Transition trigger: When entire patient journeys complete 85%+ automatically AND all departments trust the handoffs.
Phase 4: Bounded Autonomy (2028+): “AI Runs Operations Within Guardrails”
What it looks like in practice: AI agents manage entire operational categories with human supervision, not intervention. Humans focus on exceptions, strategy, and relationship work.
Real workflow example (Chronic Care Management):
Diabetic patient panel (n=500):
- Monthly: Wellness Agent texts A1C check reminder → Books labs → Results to clinician dashboard
- Quarterly: Coordination Agent schedules endo → Orders routine labs → Updates care plan
- As needed: Acute Agent detects “feeling dizzy” → Immediate escalation → Glucose check → ER if critical
Human involvement: 5% of interactions (complex cases, patient requests, quality review)
What “bounded” actually means:
- ALLOWED: Routine scheduling, reminders, data gathering, simple triage
- BLOCKED: Clinical diagnosis, medication changes, treatment decisions
- ESCALATE: High-risk symptoms, patient requests human, confidence <90%
- MONITOR: Weekly outcome reviews, monthly process audits
Success metrics:
- Operational ROI (target: 2–3x cost savings vs manual)
- Patient outcomes (target: readmission rates -20%, adherence +15%)
- Staff satisfaction (target: “I spend more time with patients” >80%)
Enabling factors (what must be true):
- Mature integrations: EHR, CRM, labs, pharmacy, payer portals (read/write)
- Proven Phase 1–3: 2+ years of reliable automation
- Strong governance: Audit trails, outcome measurement, regulatory compliance
- Clinician trust: Proven time savings + patient safety record
- Continuous learning: Agents improve from real outcomes
Common pitfalls:
- Removing humans entirely (creates brittleness)
- Scaling unproven workflows
- Ignoring regulatory evolution
“Will AI Take Over Healthcare?” (What Ops Leaders Actually Hear)
Short answer: No. AI takes over delays. The AI systems in healthcare are not given any executive decision making skills- just faster and cleverer execution of what has been thought through by healthcare providers. To see what actually get’s repllaced (PS: It’s not us), read these points:
What AI Replaces
- After-hours phone tag
- Repetitive documentation
- Form assembly and chasing
- Missed follow-up reminders
- “Where is my patient?” tracking
What AI Amplifies
- Clinician-patient face time
- Care coordinator bandwidth
- Revenue cycle speed
- Patient satisfaction
- Staff retention (less burnout)
I’ve seen ops teams go from skeptical to champions when they measure the time recovered. One clinic director told me: “My nurses went from 70% admin to 70% patient care. That’s what AI adoption looks like.”
Safety First: How Healthcare Ops Makes AI Accountable
Smart ops teams don’t deploy AI blindly. They build guardrails:
Non-Negotiables
- Audit trails: Every action logged, searchable, reviewable
- Escalation paths: Clear rules for “send to human”
- Human approval: High-risk actions require sign-off
- Data security: HIPAA, encryption, access controls
- Continuous monitoring: Weekly outcome reviews, not annual audits
The Ops Safety Checklist
- Every AI action creates a log
- Patients can always request a human
- Clinical decisions require clinician approval
- Denial rates / errors are tracked weekly
- Staff can override AI with one click
Implementation Roadmap: The 30-Day Ops Playbook
Now if you’re a healthcare professional or in any capacity involved with the domain, you must be asking – now what? How does one achieve such ‘high-tech’ systems and replace years old traditions?
Here is exactly how any one can start their journey towards being AI-assisted in healthcare:
Step 1: Find Your #1 Bottleneck (Days 1–7)
Every ops team has one workflow that keeps everyone up at night. Pick yours:
- Scheduling lines constantly busy → Deploy patient access agent
- Clinicians charting after 8 PM → Roll out ambient scribes
- Prior auth team underwater → Revenue cycle agent
- High readmission rates → Care coordination agent
Success rule: Choose the workflow where you can measure “before” vs “after” in 30 days.
Step 2: 30-Day Pilot, One Team (Days 8–37)
Start small: 1 department, 1 shift, 30 days. Track three things daily:
- Time recovered (staff self-reported)
- Patient feedback (simple 1–5 scale)
- Errors/escalations created
Hold 15-minute daily debriefs: “What worked? What failed? What needs human?”
Step 3: Connect Systems, Train Neighbors (Days 38–60)
Integrate with EHR/CRM/scheduling. Train adjacent teams on escalation paths.
Build “muscle memory” for when/how to override AI.
Step 4: Scale What Works (Day 61+)
Weekly leadership dashboard, 4 metrics only:
- Time saved per staff member
- Patient satisfaction (NPS/CSAT)
- Escalation rate (must trend down)
- Revenue impact (prior auth speed, no-show reduction)
Expand to second workflow only when first hits 80% success.
Book a 20‑minute ContactSwing demo and watch an AI agent reschedule, confirm, and document an appointment without a single manual step.
Key Takeaways
- AI agents in healthcare handle scheduling, documentation, prior auth, and follow-ups-freeing staff for patient care.
- Generative AI turns complex info into clear patient instructions and team handoffs.
- Patient care becomes more convenient: 24/7 answers, fewer delays, clear next steps.
- Ops capacity increases: Clinicians recover 1–2 hours daily. Coordinators handle more patients.
- Safety is designed in: Audit logs, human escalation, continuous monitoring.
- ROI is measurable: Track time saved, patient satisfaction, revenue speed.
AI isn’t coming to “take over” healthcare. It’s already helping ops teams deliver better care, faster. The question isn’t “should we use AI?” It’s “which workflow do we fix first?”
FAQs (What Healthcare Ops Leaders Actually Ask)
Is AI safe for patient-facing workflows?
Yes, when built with audit logs, escalation paths, and human oversight. Patients can always request a human.
Will AI replace my staff?
No. AI replaces repetitive tasks. Staff get capacity back for patient care and complex work.
What’s the fastest ROI workflow?
Patient access (scheduling/calls) and documentation. Both have clear before/after metrics.
How does AI improve patient experience?
24/7 answers, fewer repeats, clear next steps, less “lost in system” frustration.
What about HIPAA compliance?
Non-negotiable. Look for encryption, access controls, audit trails, and SOC2/HIPAA certification.
Can we start small?
Absolutely. Pilot one workflow, one team, 30 days. Measure everything.
Will clinicians resist AI?
Most don’t when they see time back. Start with documentation-universal pain point.




